Pelvic Organ Prolapse
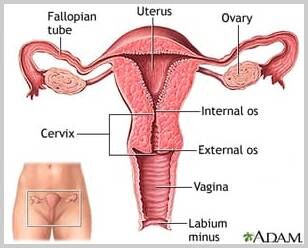
Pelvic organ prolapse or vaginal prolapse is a common condition in women, particularly as they age, occurring when a pelvic organ shifts from its normal position and begins to push against the vaginal walls. This movement causes pelvic pressure, stretching and pain. Most frequently, pelvic organ prolapse occurs after childbirth, particularly multiple children or menopause.
Pelvic organ prolapse can involve a number of different organs, including the vagina, the uterus, the bladder, the urethra, the small intestine or even the rectum. Pelvic organ prolapse is usually a benign condition but it can impair quality of life and if it worsens is can lead to increased pain and disability and may require surgical repair.
Risk Factors for Pelvic Organ Prolapse
Most commonly, pelvic organ prolapse occurs after the straining of pelvic muscles during a vaginal childbirth delivery. Risk factors for this condition include the following:
● Obesity
● Chronic cough or lung disorders
● Frequent constipation and straining to have bowel movements
● Pelvic tumors
● Low estrogen levels
● Hysterectomy
● Neuromuscular conditions or spinal cord injury
● Having multiple children, particularly close together
Symptoms of Pelvic Organ Prolapse
Women who have a pelvic organ prolapse may experience some or all of the following symptoms in various degrees:
● Frequent urination or develop incontinence (loss of urine control)
● Pain during sexual intercourse (dyspareunia)
● Pressure in the lower abdomen or against the vaginal wall
● Pulling or stretching sensation in the groin or lower back
● Constipation
● Needing to press on the back of the vaginal wall to move the bowels
● Sensation that something is protruding from the vagina
● Vaginal spotting or bleeding
● A bulge in rectum or in vagina
Diagnosis of Pelvic Organ Prolapse
The provider is usually able to diagnose this condition through a thorough pelvic examination, medical history, and review of associated symptoms. Once it is diagnosed, it is staged according to severity which can help guide treatment. Testing that may be administered to confirm a diagnosis of pelvic organ prolapse include:
● CT scan of the abdomen and pelvis
● Cystoscopy to evaluate urethra and bladder
● Fluoroscopy
● Intravenous pyelogram
● Sonogram
● Urodynamic tests
Treatment of Pelvic Organ Prolapse
Depending on the location and staging of the pelvic organ prolapse, and upon which organs are prolapsing, treatment methods may vary. It may also be guided by comorbid conditions and patient preference.
Conservative Treatment
Patients experiencing only mild symptoms may be instructed to lose weight, reduce their caffeine intake and perform Kegel exercises to strengthen their supporting vaginal muscles. Estrogen vaginal cream may be prescribed for appropriate postmenopausal women because this hormone helps to strengthen vaginal tissues, lessening atrophy of the vagina. This may prevent further prolapse and may assist the patient's comfort in using a pessary, a device designed to support the vaginal walls.
Surgery
Generally a referral is placed to gynecology or a urogynecologist. When pelvic organ prolapse cannot be controlled with lifestyle changes or the insertion of a pessary device, surgery may be required to repair one of the following:
● Vaginal wall (vaginal vault suspension)
● Urethra (urethrocele)
● Bladder (cystocele)
● Rectum (rectocele)
● Small bowel (enterocele)
In some cases, where the uterus is exerting undue pressure on the vagina, a hysterectomy may be recommended for treatment. In some rarecases, the vaginal opening is closed entirely during a procedure known as a vaginal obliteration.While it is often necessary to treat pelvic prolapse because of its tendency to worsen over time, it is usually best to treat the condition as conservatively as possible and only recommend surgery when it is necessary.
